Claims Submission & Management
- Home
- Claims Submission & Management

Claims Submission
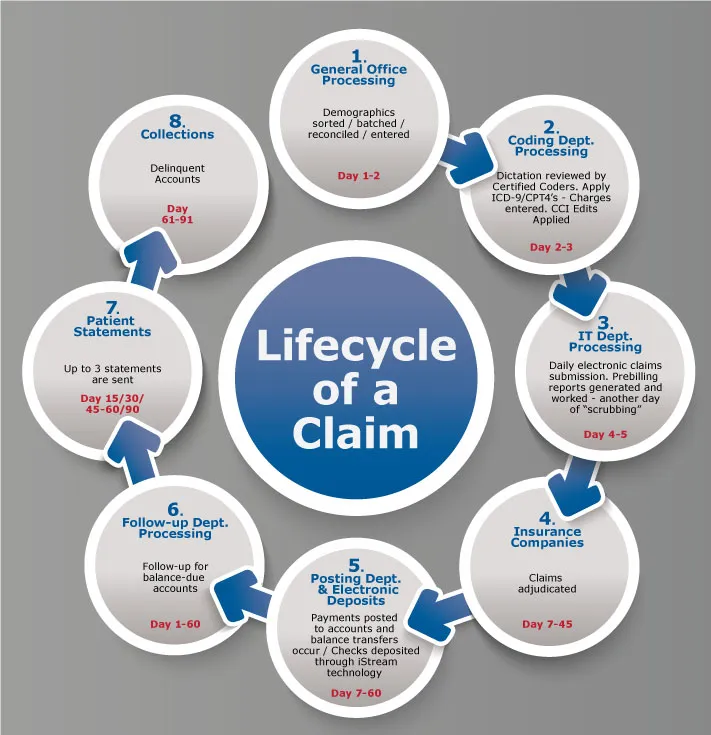
Our claims submission and management process is designed to ensure accuracy, speed, and compliance. We handle every step—from claim creation and scrubbing to timely submission and payer follow-ups. Our expert team minimizes denials by working with your system or we can recommend a system and help verify coding and patient information before submission. We track each claim through its lifecycle to ensure nothing falls through the cracks. With real-time monitoring and quick resolution of issues, we help maximize your reimbursements. Trust Olive Medical Billing Services to manage your claims with precision and care.
At Olive Medical Billing Services, our claims submission process starts with precision. We carefully verify all patient and provider information, provide guidance towards medical coding, and perform thorough claim scrubbing before submission. This attention to detail significantly reduces errors, rejections, and delays, setting the foundation for faster payments and a healthier revenue cycle.
Our team handles both electronic and paper claims, submitting them promptly to all major insurance providers and payers. We follow industry best practices and stay up to date with payer-specific guidelines to prevent unnecessary claim denials. By using advanced billing software and tools, we ensure that each claim is clean, complete, and compliant from the start.
Claims management doesn’t end at submission. We track each claim through its entire lifecycle, identifying and addressing issues as they arise. Our proactive approach includes timely follow-ups, appeals for denied claims, and communication with payers to resolve discrepancies. We are committed to minimizing aging claims and maximizing collections.
With Olive Medical Billing Services managing your claims, you gain peace of mind and more time to focus on patient care. We act as an extension of your practice, offering transparency, accountability, and results. Let us streamline your billing process and help your practice grow with dependable claims submission and management.
Comprehensive Revenue Cycle Management
We provide end-to-end revenue cycle management that covers every stage of your billing process. From patient registration and eligibility checks to claims submission, payment posting, and reporting, we handle it all. Our goal is to improve cash flow, reduce administrative burdens, and eliminate billing inefficiencies. With a proactive approach, we identify issues before they impact your revenue. Our experienced team monitors every claim closely and ensures proper follow-up. Partner with us to streamline operations and boost your financial performance.
Get Quote Now
Get a personalized quote now and discover how our billing solutions can save you time, reduce errors, and increase your revenue.
